Knee pain is a very annoying discomfort that most people unfortunately face. They can be sharp, painful, burning, throbbing, restrict the mobility of the joints, only during physical activity, or even occur at rest. However, instead of going to the doctor, many people try to eliminate them with painkillers, especially ointments, gels, or tablets of nonsteroidal anti-inflammatory drugs. Such drugs, although having anti-inflammatory properties, are unable to influence the pathogenesis of knee pain and therefore only temporarily contribute to their elimination. Therefore, they can only be considered as a means of symptomatic therapy.
But the causes of discomfort in the knee joints lie in the occurrence of various disorders, both directly in the knee and in the spine or other parts of the body. Therefore, only after determining the exact cause of the appearance can an effective treatment strategy be developed that will really help relieve the pain. To do this, you will have to go through a series of diagnostic procedures and seek expert advice, but this is the only way to really improve your well-being and avoid complications.

Cause
Knee pain can accompany many diseases, from arthrosis of the knee joints to pathologies of the lumbar, sacral spine and pelvic bones. In addition, chondropathy, arthritis, neuritis, and the like can be the cause of discomfort or even acute pain in the knee.
The obvious cause of the development of pain syndrome is a variety of injuries ranging from bruising, dislocation to ligament rupture, meniscus damage, or intraarticular fractures. But in such situations, the pain is almost always acute and occurs at the time of the collision, fall, or other traumatic factors. Therefore, in such cases, victims should contact a traumatologist to deal with the consequences of the injury.
Thus, knee pain is always a sign of a pathological process that affects the cartilage, bone, or soft tissue structures of the knee itself, or damage to the nerve that innervates it. Consider the main reasons for their appearance.
Arthrosis or gonarthrosis of the knee joints
Osteoarthritis, knee inflammation, or gonarthrosis are one of the most common causes of knee pain. This disease is characterized by the occurrence of degenerative-dystrophic processes in the cartilaginous structures of the joint, which is due to a violation of the flow of metabolic processes, the influence of traumatic factors in the past, and so on. consequence. Very often, gonarthrosis is diagnosed among the middle-aged and elderly, athletes, and those who do heavy physical work.
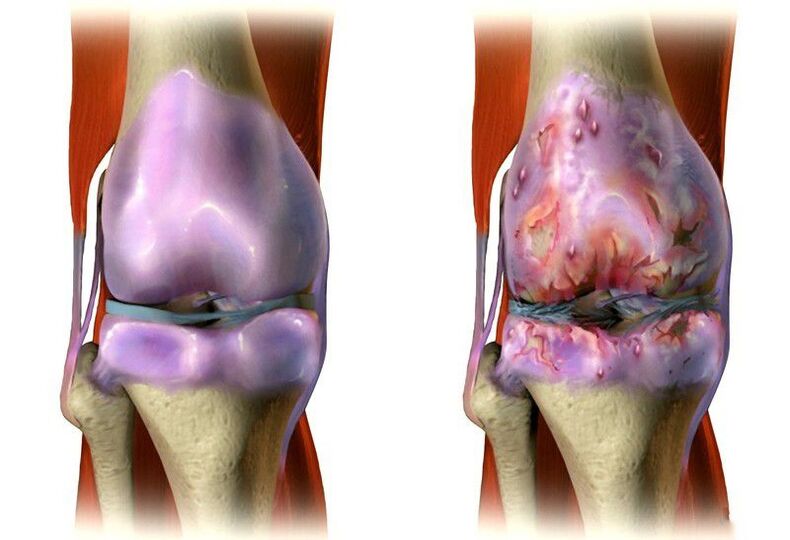
This disease is chronic, progresses slowly, and eventually leads to marked restriction of joint mobility, impaired limb support function (often both), and pain. At first they are dull, sore, pulling, and appear on the move, accompanied by a knee-jerk, especially when climbing stairs. However, in the absence of treatment, the cartilage of the knee joints is constantly worn out, leading to increased pain and presence even at rest. This is followed by destruction of the joint surfaces, which further worsens the situation and can even lead to disability.
A characteristic feature of arthrosis of the knee joints is the presence of initial pain, which requires the patients to "dissipate. " As a result, improvement can be observed within 15 to 30 minutes.
Gonarthrosis is often complicated by the addition of inflammatory processes that can affect the joint sac, ligaments, and tendons. This leads to a sharp increase in pain, the acquisition of the character of the crack, the swelling of the soft tissues and a local increase in temperature.
Spinal Disorders And Pelvic Bone Asymmetry As A Cause Of Knee Pain
At first glance, there is no connection between the lumbar spine and the knee. But in reality this is not the case. These are tightly connected by the sciatic nerve (sciatic nerve), which is the main nerve in the foot. It originates from the spine and at the same time forms fibers that protrude from the spinal cord through the natural openings in the nerve vertebrae:
- L4;
- L5;
- S1;
- S2;
- S3.
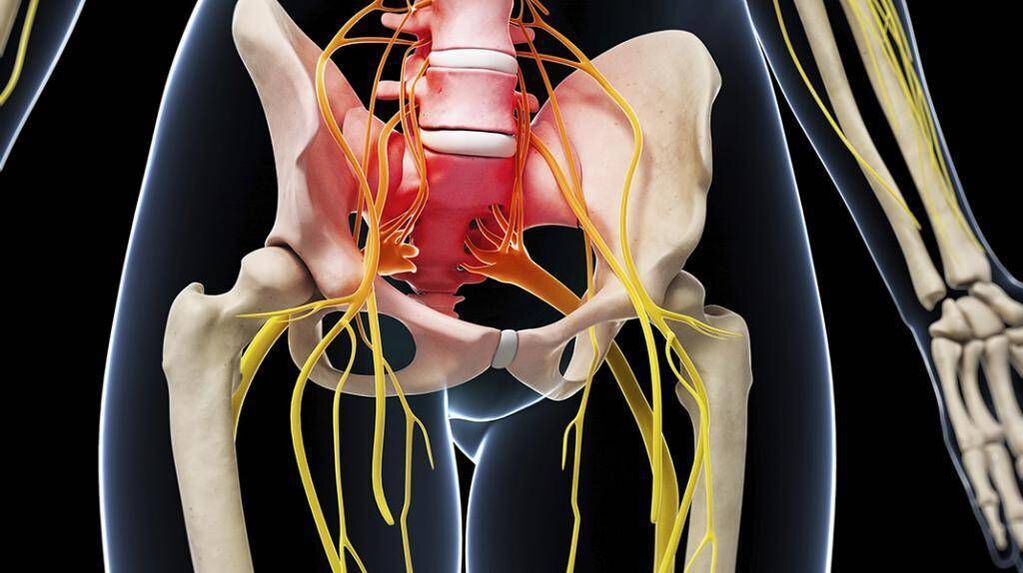
These nerves pass through the vertebrae of the same name and merge into the neural plexus at the level of the sacrum. The sciatic nerve leaves him along the back of each leg and nerves his knee. However, this nerve is responsible for its sensitive (sensory) and motor (motor) functions. Therefore, injuries at any point of transit, especially in the lumbar region, can cause pain in the knee. It is most often caused by:
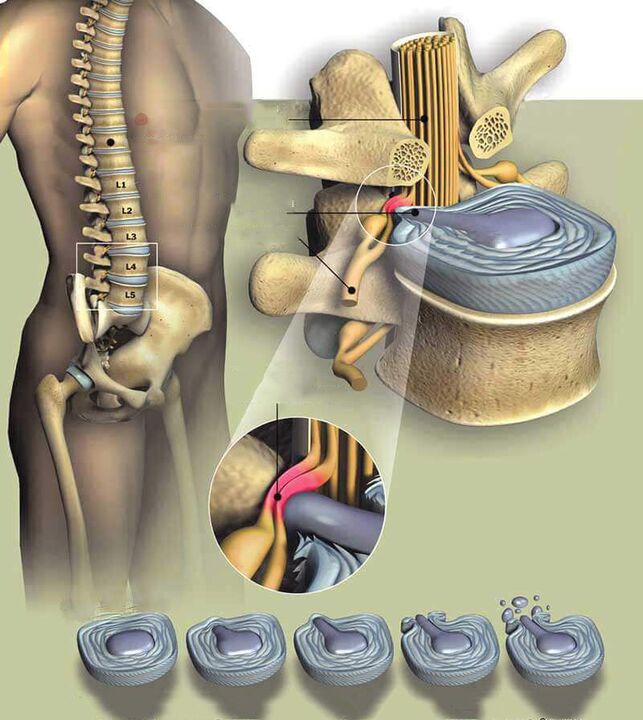
- Osteochondrosis, protrusions and intervertebral hernias. These diseases are based on degenerative-dystrophic lesions of the intervertebral discs located between almost all vertebrae. They are characterized by a systematic decrease in the height and drying of the disc, leading to a decrease in the elasticity of the structures and an increase in the risk of their tearing under load. As a result, the vertebrae move closer together, which can lead to compression of the nerve roots passing through them. If such changes occur in the lumbar region, it is possible to compress the fibers that make up the sciatic nerve and, accordingly, the appearance of knee pain. But more often, this symptom occurs when osteochondrosis complicates the protrusion (protrusion) of the intervertebral disc or its hernia (rupture of the outer shell of the disc) because protruding areas can strongly compress the roots of the spine directly in the disc. spinal canal and provokes the appearance of severe neurological complications, including pain in the knee.
- Spondylosis. It is a disease that most commonly develops in the background of osteochondrosis and is chronic. This results in an overgrowth of the surfaces of the vertebral bodies next to the intervertebral discs and the formation of osteophytes. In severe cases, the adjacent vertebrae are able to coalesce, leading to immobilization and severe compression of the nerves passing through them.
- Spondylolisthesis. This term refers to a pathology of the spine in which the upper vertebra is displaced relative to the lower vertebra. The lumbar region is most commonly affected, leading to damage to the nerves that make up the sciatic nerve.
Signs that suggest a cause of knee pain due to lumbar spine pathologies may include:
- pulling, sore, sharp pains in the lower back;
- muscle tension, thigh muscles, quadriceps, occupying the entire anterior surface of the thigh and part of the outer side;
- pain and stiffness in the hips;
- diffuse pain in the legs;
- pain in the upper thighs.
In each case, the set, nature and severity of the symptoms will be different. This is highly dependent on the individual characteristics of the body and the degree of nerve compression.
It may refer directly to sciatic nerve loss (symptoms are seen in only one limb and both at a time):
- pain in the knee, hip and lower back;
- spasms of the muscles of the back and legs;
- burns in the back of the foot;
- loss of control of bladder and intestinal function.
Violation of the function of the sciatic nerve often causes a feeling of instability in the knee, their compression. As a result, the patient complains that he cannot fully lean on his leg.
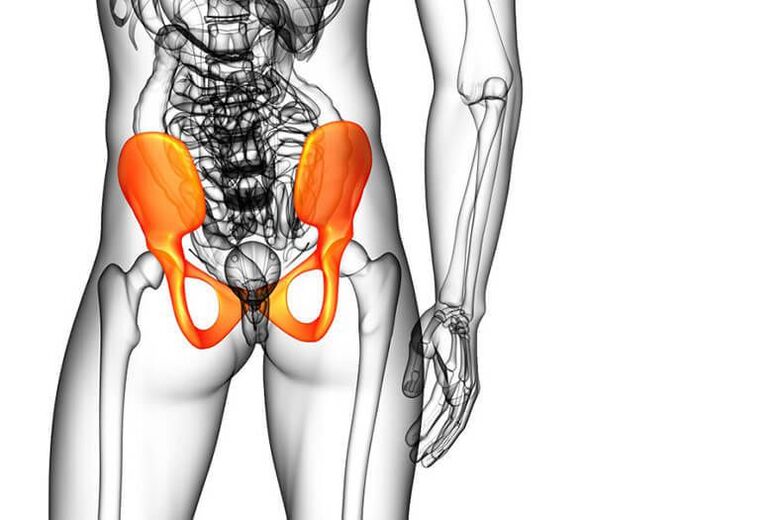
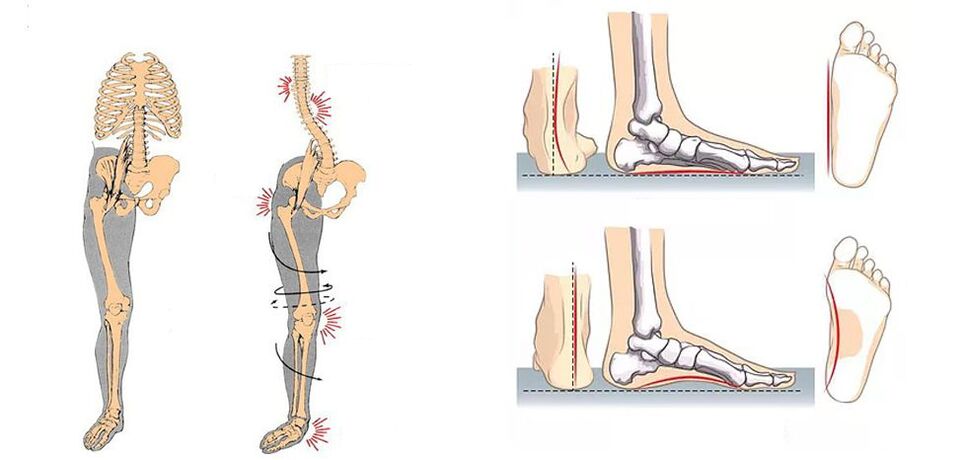
Asymmetry of the sacrum and pelvic bones can also trigger pain in the knee joint. This is due to the difference in the length of the lower limbs, which can result from the innate characteristics or curvature of the pelvis, including the background of the scoliosis. This leads to overloading of one foot and faster wear of the cartilage of the knee joint, resulting in arthrosis.
The abdominal muscles, which are connected to the pubic bone, are responsible for ensuring the stability of the pelvic bones. If they become weak due to overweight, a sedentary lifestyle, or other factors, the back muscles of the thigh are overloaded. This in turn causes an overload of the knee joint.
Pathologies of the foot and ankle
Arthrosis of the ankle joints as well as the knee may be affected. It is often diagnosed in athletes, especially ballet dancers, gymnasts, and the elderly. This leads to a violation of the biomechanics of the movements, which increases the load on the knee joint and contributes to faster wear. In such situations, the person is disturbed not only by pain in the knee but also in the ankle, which significantly affects walking due to limited movements.
Foot pathologies, especially flat feet and hallux valgus, can also cause increased strain on the knee and cause pain. These orthopedic pathologies are very common today and in most cases begin to develop in childhood and worsen in adulthood. Valgus deformity is characterized by a violation of the axis of the ankle joint due to the inward collapse of the foot. This is accompanied by increased fatigue and pain in the legs, but can also lead to knee pain later on.
Diagnostics
If you experience pain in your knee, especially if it occurs regularly or permanently, see a doctor. If the patient has recently experienced traumatic factors, they should contact an orthopedic traumatologist. In other cases, you may initially seek a consultation with a therapist. The doctor assesses the patient's condition, collects a medical history, and prescribes diagnostic procedures. This allows him to make a preliminary diagnosis and refer the patient to the professional who is most effective in helping him or her in a given case.
But you can contact a neurologist immediately if a person notices lower back pain, diffuse pain in the leg, burns on the back surface, or other symptoms described above. This will save you time and money, identify the real cause of the change in well-being as soon as possible, and start treatment. If the patient notices a change in the condition of the legs, in addition to the pain in the knee, there is also pain in the ankle joints, it is better to make an appointment with an orthopedic doctor immediately.
In any case, the doctor will study the situation in detail, assess the nature of the complaints, and refer the patient for an examination, which may include:
- laboratory tests (UAC, biochemical blood test) needed to identify signs of inflammatory processes in the body;
- X-ray of the knee in two projections (also examined by radiography if pathology of the foot or spine is suspected), which is necessary to assess the condition of the bone structures and to identify indirect signs of bone tissue. number of diseases;
- CT is used to more accurately diagnose joint diseases and to provide the most reliable assessment of their rate of death;
- Ultrasound of the knee joint for visual assessment of all structures, sizes and positions of the knee;
- MRI, which is currently the best method for diagnosing various pathologies of soft tissue structures, including cartilage cartilage and intervertebral discs.

In some cases, patients may be prescribed arthroscopy, an invasive method for diagnosing and treating pathologies of the knee joints. Usually for severe arthrosis and ligaments, meniscus, etc. necessary for traumatic injuries.
Treatment
Because there are many diseases that can manifest as knee pain, there is no single treatment strategy. In each case it develops individually, only the nature of the pathological lesions, their severity, the presence of concomitant pathologies, the individual characteristics of the patient, age, etc. Based on.
For pathologies of the spine that cause knee pain, treatment is performed under the supervision of a neurologist. If these were the consequences of arthrosis, knee, ankle joints, or other pathologies of the foot, treatment should be prescribed by an orthopedist.
When diagnosing spinal or pelvic bone pathologies, in addition to consulting a neurologist, patients may be advised to visit an endocrinologist to help resolve the problem of obesity.
All patients with spinal diseases with orthopedic pathology, including knee arthrosis, are prescribed complex treatment, which may include:
- drug therapy;
- physiotherapy;
- practical therapy;
- manual therapy.
Each measure is strictly selected according to the diagnosis and the degree of disregard for the pathological lesions. And with 2-3 degree arthrosis of the knee joints, plasmolifting is often prescribed as well.
Medical therapy
Medication usually involves 2 areas: symptomatic and etiotropic therapy. The first is to quickly improve patient well-being, eliminate knee pain and other pre-existing symptoms. The second aims to directly influence the cause of the disorder and to normalize the patient's condition in the long run.
Therefore, in most cases, patients are prescribed a drug complex:
- NSAIDs are symptomatic therapies that allow quick relief of knee, lower back, and leg pain and have an anti-inflammatory effect.
- Corticosteroids are potent anti-inflammatory drugs, indicated for severe inflammation, and are most commonly injected into the joint cavity. It is used in short courses.
- Chondroprotectors contain components that cartilage tissue uses to regenerate. They are appointed with long courses, usually lasting at least 2-3 months.
- Muscle relaxants are medications that are prescribed for muscle cramps in the back and hips, which is often the body’s reflex response to pain impulses.
- Vitamin complexes are drugs that improve the body's metabolic processes and the transmission of bioelectric nerve impulses along the nerves.
Plasmolifting
Plasmolifting is the injection of plasma from a patient's own blood directly into the affected knee joint or the soft tissues around it. Due to its saturation with platelets, cytokines and growth factors, it contributes to:
- stimulating the flow of natural regeneration processes;
- restoring the normal composition and volume of synovial fluid;
- activation of blood circulation and feeding of articular cartilage;
- elimination of inflammation;
- pain relief;
- restoring the normal range of motion of the affected joint;
- a 2-3-fold reduction in treatment time.
PRP therapy, also known as plasmolifting, is a perfect complement to the treatment of knee arthrosis and is therefore often included in the treatment regimen for this disease. It can also be used to treat osteochondrosis and injuries of the spine, in addition to drug therapy, physiotherapy, gymnastics, and other treatments.

Physiotherapy
Different types of physiotherapy can be used to treat musculoskeletal disorders that cause knee pain. They increase the effectiveness of other treatments and have a positive effect on the affected area. Physiotherapy is always prescribed in courses of 7 to 15 procedures, which are selected individually. Most often they ask for help:
- magnetotherapy;
- ultrasound therapy;
- UHF;
- phonophoresis;
- electrophoresis;
- SMT therapy or amplipulse therapy;
- vibration massage.
practice therapy
Physiotherapy practices play an important role in the treatment of pathologies of any location in the joints, especially the spine. It allows a dose increase in the range of motion as well as a stimulation of blood circulation, which leads to the activation of the nutrition of all the structural elements of the knee joints and thus contributes to their regeneration.
But it is important to choose the optimal set of exercises that is most useful in this situation and does not cause harm. Patients can be advised to perform stretching exercises that are particularly important for spinal pathologies. In addition, exercises are almost always prescribed to strengthen the musculoskeletal system. They contribute to the development of a strong muscle skeleton, which reduces the load on the affected joints and creates favorable conditions for their healing.
Physiotherapy sessions are simple and accessible to all ages, as a personalized program ensures the development of a dose that has a positive effect on the patient’s joints and eliminates practices that may be harmful. But in order to learn the methodology of each of the suggested exercises as accurately as possible, it is worthwhile to conduct the first lessons under the supervision of an instructional therapy instructor.

In the future, you can practice at home, in nature or in any other suitable place, but daily. Systematicity is one of the basic rules for the success of physiotherapy practices. Therefore, you need to add it to the list of daily activities and give it the right time - 20-30 minutes is usually enough. During classes, it is important to avoid sudden movements and haste, as this can cause pain and worsen the condition.
Manual therapy
Manual therapy is one of the key roles in the correction of pelvic asymmetry and in the treatment of spinal diseases. This includes an in-depth study of the muscles of the back, the ligaments and joints of the spine, and the pelvic region by the hand of a specialist. There are many methods and techniques for manually influencing. These are selected depending on the type and severity of the existing pathology.
Thanks to the manual therapy sessions, it is possible to:
- eliminates back pain by relieving pressure on nerve fibers;
- improves the nutrition of all structures of the spine due to the activation of blood circulation;
- increases spinal mobility;
- improves posture by eliminating spinal deformities;
- restores the normal condition of the pelvic bones and internal organs, which has a positive effect on their function.
But the most important effect of hand therapy in patients with knee pain is to eliminate compression of the sciatic nerve and the fibers that make it up. This leads to a gradual improvement in the condition and the cessation of pain syndrome and other neurological disorders.
Patients notice the first positive changes after the first treatment. Additional processes will contribute to its growth and long-term stabilization. The first procedures can be performed only after the removal of the acute inflammation using drug therapy, physiotherapy and other methods of treatment.

Thus, knee pain may indicate not only its defeat but also problems in other parts of the musculoskeletal system, especially the spine and legs. In any case, they cannot be ignored, as existing pathologies progress over time in the absence of appropriate treatment. This leads to an increase in the severity of the pain, the appearance of other unpleasant symptoms and a decrease in the quality of human life in general. Therefore, if you experience discomfort in one or both knees, consult a doctor: an orthopedist or a neurologist. Timely treatment in the early stages of the pathological changes allows them to be reversed and the joint to be restored to normal functioning, ensuring freedom of movement for many years.































